Anal fistulas are abnormal connections that form between the inside of the anal canal and the skin near the anus. They usually develop as a result of an abscess, which is a painful collection of pus caused by infection. When an abscess drains incompletely or recurs, it can create a persistent tunnel known as a fistula. Many people experience recurring pain, swelling, or discharge in the perianal area before a diagnosis is made. Anal fistulas are more common in men and can appear at any age, often following an initial episode of abscess formation. Understanding the relationship between abscesses and fistulas is crucial for effective treatment. Without proper care, a fistula can lead to chronic infections, scarring, and significant discomfort that impacts daily life.
The importance of timely repair cannot be overstated. Treating a fistula promptly after abscess formation reduces the risk of recurring infections and prevents the development of complex fistulas that are more difficult to treat. Anal fistula repair and removal procedures aim to restore normal anatomy while preserving continence. Leaving a fistula untreated often results in persistent drainage, irritation, and repeated hospital visits for abscess drainage. Beyond physical discomfort, untreated fistulas can also affect emotional and social well-being due to pain, odor, or embarrassment. Early intervention ensures better healing outcomes and lowers the chances of long-term complications. Patients are generally encouraged to seek professional evaluation at the first signs of persistent anal pain or discharge.
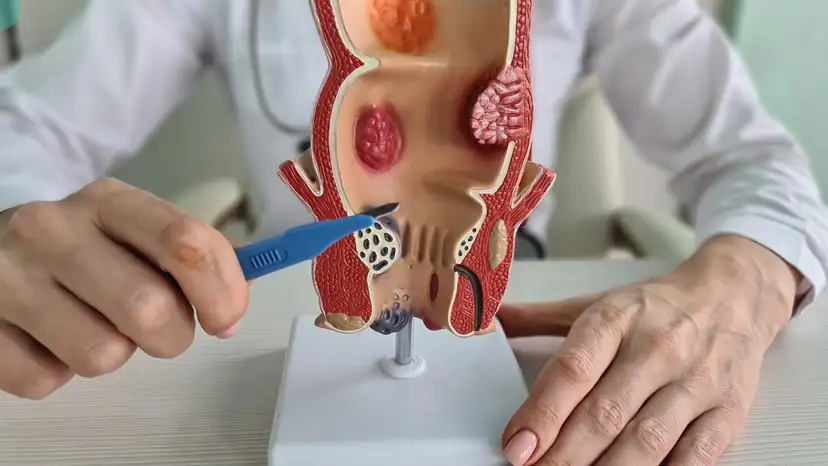
Accurate diagnosis is a critical step before any surgical intervention. Physicians typically begin with a thorough physical examination to detect openings, swelling, or tenderness around the anus. Imaging techniques, such as magnetic resonance imaging or endoanal ultrasound, provide a detailed view of the fistula’s path and its relationship to surrounding structures. Fistulas are classified into simple and complex types, which helps determine the most appropriate treatment approach. Simple fistulas are usually superficial and easier to treat, while complex fistulas may involve multiple tracts or proximity to the anal sphincter, requiring more intricate surgical planning. Correct classification reduces the risk of incomplete treatment or recurrence. Understanding the fistula’s anatomy also helps surgeons minimize complications and preserve anal function during repair.
Anal fistula repair and removal options vary depending on the type and complexity of the fistula. Fistulotomy is one of the most common procedures and involves opening the fistula tract to allow it to heal from the inside out. Fistulectomy, on the other hand, removes the entire fistula tract, which can be necessary for more complex or recurrent cases. Minimally invasive options, such as the LIFT procedure, advancement flap, or fistula plugs, are increasingly used to reduce healing time and preserve sphincter function. The choice of procedure depends on factors including the fistula’s location, the involvement of sphincter muscles, and the patient’s overall health. Surgeons weigh the benefits and potential risks of each technique to achieve long-lasting results. Proper patient selection and surgical expertise are essential for successful outcomes.
The role of anal fistula repair becomes particularly important after abscess formation. Once an abscess has been drained, the fistula may remain as an open channel, providing a pathway for bacteria and causing recurring infections. Timely repair helps close this channel, preventing further abscess formation and chronic drainage. Deciding when to perform the repair is important: some patients benefit from immediate surgery after abscess drainage, while others may need a period of healing before intervention. Repair also reduces the risk of complications like persistent pain, skin irritation, and scarring. Patients who undergo repair after abscess formation often experience faster relief from symptoms and improved quality of life. Addressing the fistula promptly ensures the infection does not recur and helps maintain anal function.
Recovery and postoperative care are essential components of successful treatment. Pain management typically includes prescribed medications and sitz baths to soothe the area and promote healing. Proper wound care, including keeping the site clean and dry, reduces the risk of infection. Dietary adjustments, such as consuming high-fiber foods, help prevent constipation and minimize strain during bowel movements. Patients are often advised to monitor for signs of infection, excessive bleeding, or unusual discharge. Regular follow-up appointments allow the surgeon to assess healing progress and address any concerns. Most patients can gradually return to normal activities while adhering to postoperative guidelines. Maintaining these practices improves healing speed and reduces the likelihood of recurrence.
Like any surgical procedure, anal fistula repair carries potential risks and complications. Infection and bleeding are possible, particularly if postoperative care is not strictly followed. There is also a small risk of sphincter damage, which can affect continence. Delayed healing or recurrence may occur if the fistula tract is complex or if underlying conditions, such as Crohn’s disease, are present. Surgeons employ careful planning and minimally invasive techniques to mitigate these risks. Understanding these possibilities helps patients prepare mentally and physically for recovery. Awareness of potential complications ensures prompt action if any issues arise during healing.
Lifestyle and preventive measures play a vital role in managing anal fistulas and abscesses. Maintaining proper perianal hygiene helps prevent bacterial infections that could lead to abscess formation. Adequate hydration and a high-fiber diet reduce the likelihood of constipation, which minimizes pressure on the healing tissue. Patients are encouraged to address any recurrent anal discomfort promptly rather than delaying care. Avoiding prolonged sitting and incorporating gentle physical activity can also promote better circulation and healing. For individuals with chronic conditions like Crohn’s disease, regular monitoring and management are crucial. These strategies work together to reduce the risk of future abscesses or fistulas.
Practical Tips for Postoperative Care
- Sit in warm sitz baths several times daily to relieve pain and promote healing
- Keep the surgical area clean and dry after bathing
- Eat a fiber-rich diet to prevent constipation and straining
- Avoid heavy lifting or strenuous activity until cleared by a doctor
- Monitor for unusual symptoms such as fever, increased pain, or swelling
- Attend all scheduled follow-up appointments for wound assessment
- Follow prescribed medications exactly as directed to prevent infection
Frequently Asked Questions (FAQ)
1. Can an anal fistula heal without surgery?
Most anal fistulas do not heal on their own and often persist or worsen without surgical intervention. Conservative treatments may temporarily manage symptoms, but surgery is usually required for complete resolution.
2. How long does recovery take after fistulotomy or fistulectomy?
Recovery times vary depending on the procedure and fistula complexity. Simple fistulotomy may heal in 4 to 6 weeks, while more complex fistulectomy could take up to 8 weeks or longer.
3. Is anal fistula repair painful?
Some discomfort is expected after surgery, but pain can be managed with medications, sitz baths, and proper wound care. Most patients experience gradual relief over the first few weeks.
4. Can fistulas recur after surgery?
Recurrence is possible, especially for complex fistulas or if underlying conditions are present. Following postoperative care instructions significantly reduces this risk.
5. How can I prevent an abscess from turning into a fistula?
Early treatment of abscesses, proper hygiene, high-fiber diet, and regular medical check-ups help prevent fistula formation. Addressing symptoms promptly is key to avoiding complications.
Takeaway
Anal fistula repair and removal play a critical role in preventing recurrent abscesses and restoring normal anal function. Timely surgical intervention, combined with proper postoperative care, minimizes complications and promotes long-term healing. Patients who maintain hygiene, follow dietary recommendations, and attend follow-ups experience improved outcomes and better quality of life. Understanding the causes, treatment options, and recovery process empowers patients to make informed decisions and regain comfort. By addressing fistulas promptly after abscess formation, it is possible to break the cycle of recurring infections and achieve lasting relief.